Welcome to PreCrack! We’re here to provide you Information about all best topics in their simplest manner that may help you to Crack UPSC CS Prelims Exam.
Naresh Soni
What is Inflammatory Bowel Disease(IBD)? – Symptoms, Causes, Treatment, Latest Research & Study 2024
Table of Contents
Introduction to Inflammatory Bowel Disease UPSC
Welcome to PreCrack! Recently, a study has been conducted by a renown institution on Inflammatory Bowel Disease (IBD) & a potential connection between infant diet and Inflammatory Bowel Disease. Due to this study, the Inflammatory Bowel Disease (IBD) is in the headlines again. This is one of the most famous types of chronic disease of gastrointestinal tract which affects millions of people worldwide.
Knowing about this disease is also crucial for those who are preparing for civil service examinations. If you are one of them & wants to know complete details about Inflammatory Bowel Disease (IBD), then in this blog, we have added a complete details about IBD UPSC.
So, let’s start-

Read Also | What is Kyasanur Forest Disease?
Why is Bowel Disease in the News? – UPSC Current Affairs on Inflammatory Bowel Disease
The news on Inflammatory Bowel Disease (IBD) gained attention due to a study revealing a potential link between infant diet and IBD development. Researchers tracked 80,000 children’s diets from Norway and Sweden, finding that a diet rich in fish and vegetables at age one correlated with a lower risk of IBD.
Conversely, a higher intake of sugar-sweetened beverages at the same age was associated with a higher risk. The study highlighted the significance of early-life dietary patterns, suggesting a potential preventive approach with a balanced diet for infants.
However, experts cautioned against generalizing findings to different cultural and geographical contexts and emphasized the need for comprehensive studies considering multiple factors influencing IBD.
Source – The Hindu
Details about Inflammatory Bowel Disease
We have added all the details about Inflammatory Bowel Disease below-
What is Inflammatory Bowel Disease (IBD)?
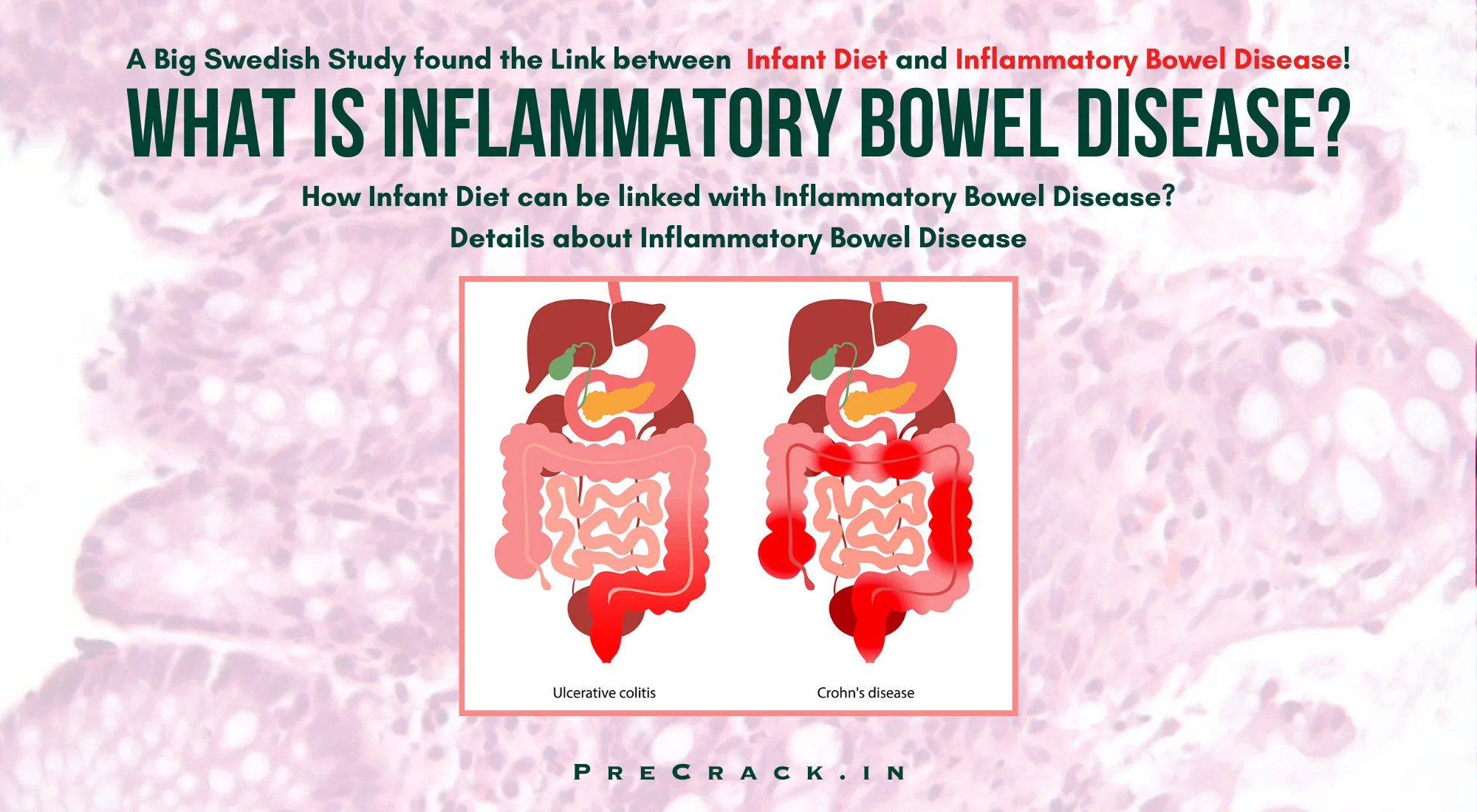
Inflammatory Bowel Disease (IBD) is an umbrella term for chronic inflammatory conditions affecting the digestive tract. The two main types of IBD are:
- Crohn’s disease: This can cause inflammation anywhere along the digestive tract, from the mouth to the anus. It typically involves deeper layers of the bowel wall and often presents with patchy areas of inflammation.
- Ulcerative colitis: This inflames the inner lining of the large intestine (colon) and rectum, usually in a continuous way from the rectum upwards.
Epidemiology of Inflammatory Bowel Disease
The exact number of IBD patients in India is difficult to determine due to variations in diagnostic practices and disease reporting. Estimates range from 0.27 million to 1.4 million people.
In 2013, Inflammatory Bowel Disease (IBD) caused 51,000 global deaths, a rise from 55,000 in 1990. The surge in IBD incidence post-World War II correlates with increased global meat consumption, suggesting a potential link to animal protein intake.
Environmental factors like smoking, air pollution, greenspace availability, urbanization, and Westernization have been associated with both increased and decreased IBD risk. Europe witnesses a rising trend in IBD cases, while Asia experiences a steady increase, likely influenced by dietary and environmental shifts.
In the UK, approximately 0.8% of the population has IBD, and in Canada, around 0.7% (270,000 people) are affected, with projections estimating a rise to 1% (400,000 people) by 2030. These statistics highlight the evolving global landscape of IBD prevalence and the multifaceted factors contributing to its epidemiology.
Signs & Symptoms of IBD
IBD symptoms can vary depending on the type and severity of the disease, the location of inflammation in the digestive tract, and whether the individual is experiencing a flare-up or remission. However, some common signs and symptoms include:
Gastrointestinal

- Abdominal pain and cramping: This is a hallmark symptom of IBD and can be constant or come and go in waves. The location of the pain may vary depending on the affected area of the digestive tract.
- Diarrhea: Frequent, loose stools are another common symptom, and they may be bloody in some cases.
- Urgency to have a bowel movement (urgency): This refers to a sudden and strong need to use the bathroom, which can be quite distressing.
- Rectal bleeding: Blood in the stool can range from bright red streaks to dark, tarry stools.
- Mucus in stool: The presence of mucus in the stool can indicate irritation and inflammation in the digestive tract.
- Incontinence: In severe cases, individuals may experience fecal incontinence, meaning they lose control of their bowels.
General
- Weight loss: This can occur due to decreased appetite, malabsorption of nutrients, or frequent diarrhea.
- Fatigue: Feeling tired and lacking energy is a common symptom of IBD, even when not experiencing a flare-up.
- Fever: A low-grade fever may be present, especially during a flare-up.
- Anemia: Iron deficiency anemia is common in IBD due to blood loss. Symptoms of anemia can include fatigue, pale skin, shortness of breath, and dizziness.
Less common symptoms
- Nausea and vomiting: These are less frequent but can occur in some individuals with IBD.
- Mouth sores: Canker sores or other mouth sores may develop in some cases.
- Joint pain and arthritis: Inflammation in the joints can occur outside the digestive tract in some individuals with IBD.
- Skin problems: Skin rashes, such as erythema nodosum (red, painful nodules) or pyoderma gangrenosum (painful ulcers), can develop in some cases.
- Delayed growth in children: Children with IBD may experience stunted growth and development due to malnutrition.
Different types of Conditions
Inflammatory Bowel Disease (IBD) encompasses two main types of conditions: ulcerative colitis and Crohn’s disease. Both conditions involve chronic inflammation of the digestive tract, but they have distinct characteristics:
1. Ulcerative Colitis

- Affected Area: Primarily the colon (large intestine) and rectum.
- Characteristics: Continuous inflammation of the innermost lining of the colon, leading to ulcers and sores.
- Symptoms: Diarrhea, abdominal pain, rectal bleeding, weight loss, fatigue.
- Complications: Severe cases may lead to toxic megacolon, perforation of the colon, or an increased risk of colon cancer.
2. Crohn’s Disease

- Affected Area: Can affect any part of the digestive tract from the mouth to the anus, often involving the small intestine.
- Characteristics: Inflammation occurs in patches, not continuous, and can extend through multiple layers of the bowel wall.
- Symptoms: Abdominal pain, diarrhea, weight loss, fatigue, complications like fistulas (abnormal connections between organs) and strictures (narrowing of the intestine).
- Complications: Can lead to complications outside the digestive tract, such as arthritis, skin problems, and inflammation in the eyes.
3. Indeterminate Colitis
- Some individuals may exhibit features of both ulcerative colitis and Crohn’s disease, making it challenging to definitively diagnose the specific type of IBD. In such cases, the term “indeterminate colitis” is used.
Causes of IBD
IBD arises from the intricate interplay of genetic and environmental factors, impacting immunological responses and causing inflammation in the intestine. While genetic predisposition and environmental triggers contribute, the complex relationship between diet, bile acids, gut microbiota, breaches in the intestinal barrier, and oxidative stress plays a pivotal role in the pathogenesis of IBD.
Genetic Factors
- Genetic predisposition plays a role in IBD development.
- Individuals with a family history of IBD have a higher risk.
Environmental Factors
Diet: A complex interplay exists between diet and IBD.
- Studies suggest associations between IBD and diets high in animal protein and sugar.
- Gluten sensitivity, common in IBD, is linked to flare-ups.
Bile Acids: Emerging evidence implicates bile acids in IBD.
- Altered bile acid patterns are observed in IBD patients.
Microbiota: The gut microbiota, comprising trillions of microorganisms, differs in IBD patients.
- Dysbiosis, characterized by an imbalance in beneficial and harmful bacteria, is more pronounced in Crohn’s disease.
- Certain bacteria contribute to IBD development, while others, like B. fragilis, play a protective role.
Breach of Intestinal Barrier
- Loss of integrity in the intestinal epithelium is a key factor in IBD pathogenesis.
- Dysfunctional innate immune responses and abnormal signaling through toll-like receptors contribute to inflammation.
- Changes in the microbiota composition induce an inappropriate immune response, leading to damage and breaches in the intestinal barrier.
Oxidative Stress and DNA Damage
- Oxidative stress and DNA damage are implicated in IBD pathophysiology.
- Increased oxidative DNA damage, measured by markers like 8-OHdG, is observed in inflamed mucosa of IBD patients.
Pathophysiology
- Cytokine Response:
- Crohn’s disease is associated with Th17 cytokine responses.
- Ulcerative colitis is vaguely associated with Th2 responses.
Diagnosis of IBD – Diagnosing Inflammatory Bowel Disease (IBD)
Diagnosing IBD can be a multi-step process because there is no single definitive test. Doctors rely on a combination of methods to reach an accurate diagnosis, which typically involves:
1. Medical history and physical exam
- Your doctor will discuss your medical history in detail, including your current symptoms, past medical conditions, family history of IBD, and lifestyle habits.
- During the physical exam, your doctor will check for signs of inflammation, such as abdominal tenderness or mass, and assess your general health.
2. Laboratory tests
- Blood tests: These can evaluate for anemia, inflammation markers, and autoimmune issues.
- Stool tests: These can check for the presence of white blood cells, blood, parasites, or bacteria, which can indicate inflammation or infection.
3. Imaging tests
- X-rays and barium X-rays: While not definitive for IBD, these can help rule out other potential causes of your symptoms, like blockages or bowel perforation.
- CT scan or MRI: These provide detailed images of your digestive tract and can be helpful in identifying inflammation, narrowing, or fistulas (abnormal connections) in the bowel.
- Capsule endoscopy: This involves swallowing a small capsule with a camera that takes pictures of the entire small intestine, helpful when other methods are inconclusive.
4. Endoscopy
- Colonoscopy: This procedure involves inserting a long, flexible tube with a camera through the anus to examine the entire colon and rectum. During a colonoscopy, tissue samples (biopsies) can be taken for further examination under a microscope to look for signs of inflammation and distinguish between different types of IBD, like ulcerative colitis and Crohn’s disease.
- Upper endoscopy: This procedure examines the upper part of the digestive tract, including the esophagus, stomach, and duodenum (first part of the small intestine). This may be necessary if symptoms suggest inflammation in these areas.
5. Biopsy
Tissue samples obtained during endoscopy are examined under a microscope by a pathologist to identify abnormal changes in the cells, indicative of inflammation or specific features of IBD.
Treatment of Inflammatory Bowel Disease
While there is no cure for IBD, various treatment options can help manage symptoms, control flare-ups, and improve quality of life. The specific treatment approach will depend on several factors, including:
Type of IBD: Ulcerative colitis and Crohn’s disease have different treatment strategies.
- Severity of the disease: Mild, moderate, and severe cases require different treatment approaches.
- Individual needs and preferences: Each person’s needs and preferences regarding medications and interventions should be considered.
Here’s a detailed breakdown of the main treatment categories for IBD:
1. Medications
- Aminosalicylates: These are anti-inflammatory medications commonly used to treat mild to moderate IBD and maintain remission. Examples include mesalamine (Asacol, Lialda), sulfasalazine (Azulfidine), and balsalazine (Colazal).
- Corticosteroids: These powerful anti-inflammatory medications are used to control severe flare-ups and suppress inflammation rapidly. However, due to potential side effects, they are typically used for short periods and not for long-term management. Examples include prednisone and budesonide.
- Immunomodulators: These medications work by suppressing the overactive immune response that contributes to inflammation in IBD. They are often used to maintain remission after achieving control with corticosteroids or in cases where corticosteroids are not effective or well-tolerated. Examples include azathioprine (Imuran) and mercaptopurine (Purinethol).
- Biologics: These are newer medications that target specific proteins involved in the inflammatory response. Biologics are often used for moderate to severe IBD, particularly when other medications haven’t been effective. Examples include adalimumab (Humira), infliximab (Remicade), and vedolizumab (Entyvio).
- Antibiotics: These can be used to treat specific infections that may be associated with IBD, such as pouchitis (inflammation of the ileal pouch after surgery).
2. Diet and lifestyle modifications
- Dietary changes: Following a specific diet plan can help manage symptoms and improve overall well-being. This may involve avoiding certain foods that trigger symptoms, eating smaller and more frequent meals, and staying hydrated. A registered dietitian can help create a personalized dietary plan based on your individual needs.
- Smoking cessation: Smoking is a known risk factor for developing and worsening IBD. Quitting smoking significantly improves disease outcomes and helps control symptoms.
- Stress management: Stress can exacerbate IBD symptoms. Therefore, practicing stress management techniques like yoga, meditation, or deep breathing exercises can be beneficial.
- Exercise: Regular physical activity can help improve overall health and well-being, maintain healthy weight, and potentially reduce inflammation. However, it’s crucial to choose appropriate exercises and adjust intensity based on your individual condition.
3. Surgery
While not a first-line treatment, surgery may be necessary in some cases of IBD, such as:
- Intractable complications: Surgery may be needed to address complications like severe bleeding, bowel perforation, or fistulas (abnormal connections between the bowel and other organs).
- Bowel obstruction: Blockage of the bowel due to inflammation or scar tissue may necessitate surgery to remove the affected portion.
- Ulcerative colitis: In severe cases of ulcerative colitis, colectomy (removal of the colon) may be considered, followed by creation of an ileostomy (an opening in the abdomen to allow waste to exit) or ileal pouch anal anastomosis (IPAA, where a pouch is created from the small intestine to function like a rectum).
Prognosis of IBD
The prognosis of IBD generally varies depending on several factors, including:
- Type of IBD: Ulcerative colitis and Crohn’s disease have slightly different outlooks.
- Severity of the disease: Individuals with mild to moderate disease typically have a better prognosis compared to those with severe cases.
- Age of onset: Early diagnosis and treatment usually lead to a better prognosis.
- Response to treatment: Individuals who respond well to medication and lifestyle changes tend to have a more favorable prognosis.
- Presence of complications: Complications like bowel obstruction or fistulas can worsen the prognosis.
Here’s a breakdown of the general prognosis for IBD:
- Overall, individuals with IBD can lead full and productive lives with proper management.
- IBD is not typically life-threatening, and mortality rates have decreased significantly in recent years due to improved treatment options.
- Most individuals with IBD experience periods of remission (no symptoms) alternating with flare-ups (increased symptoms).
- The goal of treatment is to control symptoms, prevent flare-ups, and improve quality of life.
- While there is no cure for IBD, many people achieve long-term remission with appropriate treatment and lifestyle modifications.
However, it’s important to be aware of some potential challenges:
- IBD is a chronic condition requiring long-term management.
- Flare-ups can be disruptive to daily life and work or school activities.
- Certain complications can arise in some cases, requiring additional medical intervention.
- Some individuals with severe IBD may need surgery to address complications or improve their quality of life.
Latest Research on Inflammatory Bowel Disease – Latest News – Recent Updates
We can understand the latest research on IBD through these following 10 points:
1. Infant Diet Impact
A large Swedish study tracked over 80,000 children, revealing a link between infant diet and Inflammatory Bowel Disease (IBD) development.
2. Protective Factors
Children with a high intake of fish and vegetables at one year showed a lower risk of IBD in the future.
3. Risk Factors
Higher consumption of sugar-sweetened beverages at the same age correlated with an increased risk of IBD.
4. Longitudinal Study Design
Researchers followed dietary habits from infancy to adolescence in Norway and Sweden, emphasizing the study’s comprehensive and long-term approach.
5. Gut Microbiome Role
The study suggests the developing gut microbiome may play a key role in the age-dependent relationship between diet and IBD.
6. Database Utilization
Utilizing ABIS and MoBa databases, researchers examined a cohort of 81,280 children, enhancing the study’s statistical robustness.
7. Incidence Rates
The study revealed IBD incidence rates of 32 per 100,000 person-years in ABIS and 22 per 100,000 person-years in MoBa databases.
8. Statistical Predictions
Data analysis involved scoring diet quality and assessing the frequency of intake for various food categories, enabling statistical predictions of later IBD risk.
9. Early Intervention Suggestions
Gastroenterologist Ashwin Ananthakrishnan suggests a “preventive” diet for infants, including adequate dietary fiber, fish intake, minimal sugary beverages, and a preference for fresh foods.
10. Study Implications and Considerations
The study’s strength lies in its prospective investigation, but caution is advised in generalizing results globally, emphasizing the need for diverse settings and accounting for confounding factors in future research.
Key Facts about IBD UPSC
We have added all major facts about IBD / Inflammatory Bowel Disease below-
| Key Fact | Description |
| Name | IBD |
| Full Form | Inflammatory Bowel Disease |
| Family | Chronic inflammatory diseases |
| Scientific Facts | Autoimmune or immune-mediated condition causing chronic inflammation of the digestive tract |
| Types | – Ulcerative Colitis (UC): Affects the inner lining of the colon and rectum. – Crohn’s Disease (CD): Can affect any part of the digestive tract from mouth to anus. |
| Symptoms/Signs | – Abdominal pain and cramping – Diarrhea, often bloody – Urgent need to have a bowel movement (urgency) – Weight loss – Fatigue – Anemia – Fever |
| Causes | Unknown; combination of genetic, environmental, and immune system factors suspected. |
| Diagnosis | – Medical history and physical exam – Blood tests – Stool tests – Imaging tests (X-rays, CT scans, endoscopy) |
| Treatment | – Medications (anti-inflammatory drugs, immunomodulators, biologics) – Diet and lifestyle modifications – Surgery (in some cases) |
| Mortality Rate | Generally low with proper treatment; complications can increase risk |
| Best Medicines | Use only under specialists guidance: Aminosalicylates, Antibiotics, Infliximab, Certolizumab, and adalimumab, Mirikizumab, Anti-integrin therapy |
| Best Hospitals for IBD in India | – All India Institute of Medical Sciences (AIIMS) – Sir Ganga Ram Hospital – Medanta – The Indus Valley Hospital – Apollo Hospitals (various locations) |
| History in India | – Increasing prevalence; considered a “Western disease” historically, but now rising in India. – Regional variations in prevalence of UC and CD. |
| More | – IBD is a lifelong condition requiring long-term management. – Early diagnosis and treatment are crucial. – Regular follow-up with a healthcare professional is essential. |
FAQs on IBD – UPSC Questions about IBD
Question-1: What did the recent Swedish study investigate?
Answer. The study explored the link between infant diet and the development of Inflammatory Bowel Disease (IBD) by tracking over 80,000 children’s dietary habits from infancy to adolescence.
Question-2: What dietary factors were associated with a lower risk of IBD in children?
Answer. High intake of fish and vegetables at one year of age was linked to a lower future risk of developing IBD.
Question-3: Which dietary factor showed an increased risk of IBD in children?
Answer. Higher intake of sugar-sweetened beverages at the same age was associated with an elevated risk of Inflammatory Bowel Disease.
Question-4: How long did the researchers follow the participants in the study?
Answer. The study tracked children’s dietary habits from the first year of life through adolescence in Norway and Sweden.
Question-5: What role did the gut microbiome play in the study’s findings?
Answer. The study suggests that the developing gut microbiome may be a crucial factor in the age-dependent relationship between early-life diet and IBD.
Question-6: Which databases were utilized in the research, and why are they significant?
Answer. ABIS and MoBa databases were used, providing a robust dataset with a cohort of 81,280 children, enhancing the study’s statistical strength.
Question-7: What were the IBD incidence rates revealed in the study?
Answer. The study found IBD incidence rates of 32 per 100,000 person-years in ABIS and 22 per 100,000 person-years in MoBa databases.
Question-8: How did researchers analyze the impact of early-life diet on later IBD risk?
Answer. Researchers assigned a score to diet quality, recorded the frequency of food intake, and used statistical tests to predict later IBD risk.
Question-9: What cautionary notes were provided regarding the study’s generalization?
Answer. The study’s strength lies in its prospective investigation, but caution is advised in generalizing results globally, emphasizing the need for diverse settings and accounting for confounding factors in future research.
Question-10: What is Inflammatory Bowel Disease (IBD)?
Answer. IBD refers to disorders where the digestive tract’s lining is inflamed, with two main types: ulcerative colitis affecting the large intestine and rectum, and Crohn’s disease primarily impacting the small intestine.
Question-11: What factors are known to cause or worsen IBD?
Answer. Diet, age, family history, smoking, certain medications, and changing diet patterns are reported factors influencing IBD.
Question-12: How can changing diet patterns affect IBD prevalence?
Answer. Studies suggest that shifts in diet patterns, such as increased consumption of processed foods, can impact the prevalence of IBD.
Question-13: What did a 2023 study in The Lancet attribute to higher IBD incidence in rural Telangana?
Answer. The study linked the increased incidence of IBD in rural Telangana to greater availability and consumption of processed foods.
Question-14: Is there a connection between early-life diet and the risk of developing IBD?
Answer. Recent research indicates that the diet of infants as young as one year old can influence the future risk of developing IBD.
Question-15: What are the two main types of IBD disorders?
Answer. Ulcerative colitis, affecting the large intestine and rectum, and Crohn’s disease, primarily impacting the small intestine.
Question-16: What did the Gut paper’s authors suggest regarding early-life diet for infants?
Answer. The authors recommended a “preventive” diet for infants, including adequate dietary fiber, fish intake, minimal sugary beverages, and a preference for fresh foods.
Question-17: What databases were used in the Gut paper’s research?
Answer. The study utilized the All Babies in Southeast Sweden (ABIS) and Norwegian Mother, Father and Child Cohort (MoBa) databases.
Question-18: How does the gut microbiome change through infancy, according to the Gut paper?
Answer. The gut microbiome undergoes significant changes during the first year and stabilizes by the time the infant is two to three years old.
Question-19: What cautionary notes were provided about generalizing the study’s results?
Answer. The researchers advised caution in generalizing the results globally, emphasizing the need for replication in diverse settings and considering cultural and lifestyle differences.
Question-20: What preventive measures for infants did the gastroenterologist suggest based on the findings?
Answer. Gastroenterologist Ashwin Ananthakrishnan recommended a “preventive” diet including adequate dietary fiber, fish intake, minimal sugary beverages, and a preference for fresh foods.



2 thoughts on “What is Inflammatory Bowel Disease(IBD)? – Symptoms, Causes, Treatment, Latest Research & Study 2024”
Comments are closed.