What is Cervical Cancer? – Everything You Need to Know – 10 Key Facts – UPSC Questions
Table of Contents
Introduction to Cervical Cancer UPSC
Recently, A known social media influencer & actress named Poonam Panday has faked her death on 2nd of February 2024 due to awareness about Complications of Cervical Cancer.
This sadden news have put the Cervical Cancer to the headlines. Now, for the education, this topic named Cervical Cancer is become important for us to know about.
If you are also unaware of Cervical Cancer & Its complications, Symptoms, Signs, Treatment, Diagnosis and Statistics, then in this blog, we will provide you all this.
If you are also looking for the same information, then this blog will help you by providing In & Out information about Cervical Cancer.
So, let’s start-
Read Also | 80 Ramsar Sites in India
Why Cervical Cancer is in news? – Cervical Cancer UPSC
The tragic death of renowned Actress and social media influencer Poonam Panday on February 2, 2024, due to cervical cancer has brought attention to the disease.
Her untimely demise underscores the importance of awareness, regular screenings, and early detection in the fight against cervical cancer, sparking discussions and raising awareness in the media.
What is Cervical Cancer? – What is Cervical Cancer UPSC?
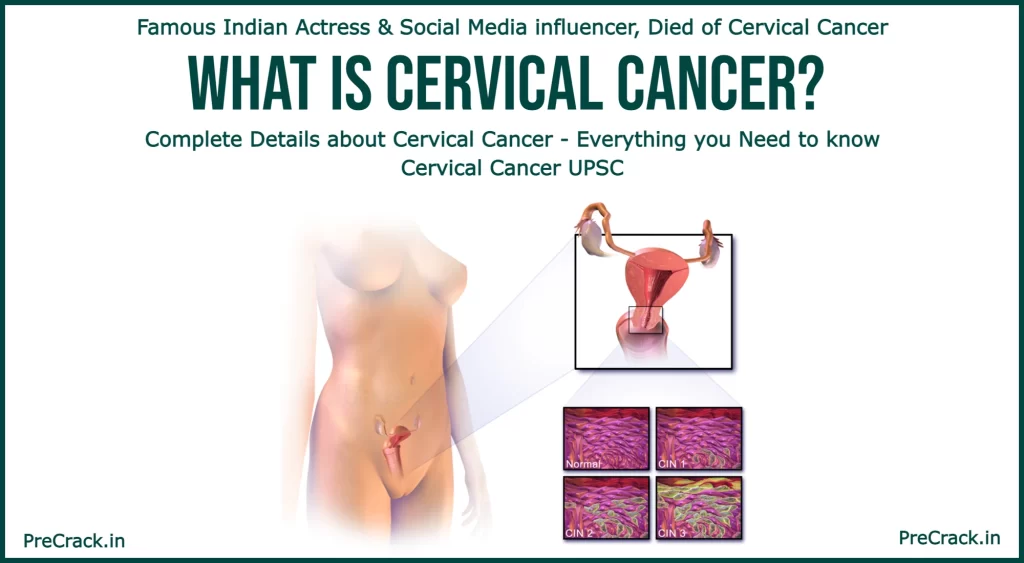
Cervical cancer is a type of cancer that starts in the cervix, the lower part of the uterus. It occurs when abnormal cell growth invades nearby tissues. Early stages often show no symptoms, but later signs include unusual vaginal bleeding, pelvic pain, or discomfort during sex.
Human papillomavirus (HPV) infection, especially types 16 and 18, is the primary cause. Other factors like smoking, weakened immune system, and genetic factors also contribute. Regular screenings, such as Pap tests, aid in early detection, and HPV vaccines can prevent some cases. Treatment may involve surgery, chemotherapy, and radiation. Early detection significantly impacts survival rates. Worldwide, cervical cancer is a significant health concern, with most cases occurring in developing countries.
Source: Wikipedia
History of Cervical Cancer UPSC – Cervic Cancer History
The History of Cervical Cancer mainly acknowledged around 400 BCE. We have listed this history below-
- Around 400 BCE: Hippocrates acknowledged cervical cancer’s incurability.
- 1925: Introduction of the colposcope by Hinselmann.
- 1928: Pioneering of the technique bearing his name by Papanicolaou.
- 1941: Onset of Pap test screening by Papanicolaou and Traut.
- 1946: Devising the Aylesbury spatula for efficient Pap test sampling.
- 1951: Emergence of HeLa, the inaugural in-vitro cell line from cervical cancer.
- 1976: Identification of HPV DNA in cervical cancer by Harald zur Hausen and Gisam.
- 1988: Establishment of the Bethesda System for Pap result reporting.
- 2006: FDA approval for the first HPV vaccine.
- 2015: Proven efficacy of HPV vaccine in shielding against infection at diverse body sites.
- 2018: Recognition of single-dose protection potential with the HPV vaccine.
In the early 20th century, epidemiologists recognized cervical cancer’s correlation with characteristics of a sexually transmitted disease. Historical research disclosed connections to factors such as profession, marital status, and viral infections. The revelation of HPV and subsequent vaccine development marked pivotal strides in cervical cancer prevention. In 2020, the World Health Organization devised a strategy aiming to eradicate cervical cancer by 2050 through vaccination, screening, and treatment interventions.
Warning Signs of Cervical Cancer – Symptoms of Cervical Cancer
From the start or 0 stage, you may not find any symptom of it, but later, this shows some bizarre symptoms. We have added them below-
1. Early Stages (May be asymptomatic)
- Vaginal bleeding
- Contact bleeding (commonly after sexual intercourse)
- Rarely, a vaginal mass
- Moderate pain during sexual intercourse
- Vaginal discharge
2. Advanced Disease (Additional Symptoms)
- Loss of appetite
- Weight loss
- Fatigue
- Pelvic pain
- Back pain
- Leg pain
- Swollen legs
- Heavy vaginal bleeding
- Bone fractures
- Rarely, leakage of urine or feces from the vagina
3. General Indicators of Concern
- Metastases may be present in the abdomen, lungs, or elsewhere in advanced stages.
- Bleeding after douching or a pelvic exam is a common symptom.
Causes of Cervical Cancer
The main cause of Cervical Cancer is HPV Infection. But there are many other causes. We have listed few of main causes of Cervical Cancer below-
1. HPV Infection
- Most cases of HPV-infected cells heal on their own, but persistent infection can lead to invasive cancer.
- HPV types 16 and 18 cause 75% of global cervical cancer cases; 31 and 45 contribute to another 10%.
- Women with multiple sexual partners, or partners with multiple partners, face a higher risk.
2. HPV Strains and Genital Warts
- Of the 150-200 known HPV types, 15 are high-risk, three are probable high-risk, and 12 are low-risk.
- Genital warts, caused by various HPV strains, are generally unrelated to cervical cancer, but multiple strains may coexist.
3. Smoking
- Active and passive cigarette smoking increases cervical cancer risk, especially among HPV-infected women.
- Smoking contributes directly by increasing the chances of cervical intraepithelial neoplasia (CIN3) and indirectly by aiding HPV development.
4. Oral Contraceptives
- Long-term use of oral contraceptives is associated with increased cervical cancer risk in HPV-infected women.
- Usage for 5 to 9 years triples the incidence of invasive cancer, and 10 years or longer raises the risk fourfold.
5. Multiple Pregnancies
- Having many pregnancies increases the risk of cervical cancer.
- Among HPV-infected women, those with seven or more full-term pregnancies have about four times the risk compared to those with no pregnancies and two to three times the risk compared to those with one or two full-term pregnancies.
Types of Cervical Cancer – Cervical Cancer Types UPSC
Now you may wonder if there is any type of it but, Yes, there are several types of cervical cancer, with the two main types being squamous cell carcinoma and adenocarcinoma. These types differ based on the cells where the cancer begins:
1. Squamous Cell Carcinoma
- This is the most common type, accounting for approximately 80-85% of cervical cancer cases.
- It originates in the squamous epithelial cells lining the cervix.
2. Adenocarcinoma
- Adenocarcinoma makes up about 15% of cervical cancer cases.
- It starts in the glandular cells of the cervix, which produce mucus.
3. Other Rare Types
- Adenosquamous carcinoma: A combination of squamous and glandular cell features.
- Small cell carcinoma: A less common and more aggressive type.
- Neuroendocrine tumor, Glassy cell carcinoma, and Villoglandular adenocarcinoma are some uncommon subtypes.
Diagnosis of Cervical Cancer
Its not impossible to have Diagnosis of Cervical Cancer. We have listed the Diagnosis below-
1. Screening and Limitations
- The Pap test is a screening tool but can produce false negatives in up to 50% of cases.
- Cost constraints limit Pap tests in some regions globally.
2. Biopsy and Confirmation
- A biopsy, often through colposcopy, confirms cervical cancer or precancer.
- Colposcopy involves magnified visual inspection with acetic acid solution, aided by staining with Lugol’s iodine.
- Biopsy devices like punch forceps are used, and colposcopic impressions contribute to the diagnosis.
- Further procedures include loop electrical excision and cervical conization for severe cervical intraepithelial neoplasia.
3. Imaging for Comprehensive Assessment
- Medical imaging (ultrasound, CT scan, MRI) is often conducted before biopsy to rule out other causes.
- Imaging detects mass heterogeneity on the cervix, evaluating tumor spread and impact on adjacent structures.
4. Precancerous Lesions
- Cervical intraepithelial neoplasia (CIN) signifies abnormal cell development on the cervix due to HPV.
- Diagnosed through routine Pap smear examination or colposcopy.
- Graded as CIN1 (mild), CIN2 (moderate), and CIN3 (severe), with CIN2 and CIN3 now combined as CIN2/3.
5. Cancer Subtypes
- Histologic subtypes include squamous cell carcinoma (80–85%), adenocarcinoma (15%), adenosquamous carcinoma, small cell carcinoma, neuroendocrine tumor, glassy cell carcinoma, and villoglandular adenocarcinoma.
- Squamous cell carcinoma, although most common, has seen an increased incidence of adenocarcinoma.
6. Staging
- Cervical cancer is staged by the FIGO system, based on clinical examination.
- Stages range from 1A to 4B, incorporating various diagnostic methods, including imaging and pathological techniques, for comprehensive staging.
How to Prevent Cervical Cancer
However, there are a few factors that can’t be prevented to have cervical cancer. But, we can try to prevent Cervical cancers by few doings…
1. Screening
- Regular Pap tests (Papanicolaou test) significantly reduce cervical cancer cases and mortality.
- Liquid-based cytology may enhance the effectiveness of Pap tests by reducing inadequate samples.
- Pap test screenings every three to five years, along with appropriate follow-up, can lower cervical cancer incidence by up to 80%.
- Abnormal cells known as cervical intraepithelial neoplasia (CIN) detected in Pap tests can be further examined through colposcopy.
- Personal invitations and educational materials are effective strategies to encourage women to undergo screening.
- Screening initiation age ranges from 20 to 30, depending on population burden and available resources.
2. Barrier Protection
- Barrier protection, including condom use during sexual intercourse, decreases the risk of transmitting HPV but does not eliminate it.
- Condoms may provide additional protection against genital warts and other sexually transmitted infections.
3. Vaccination
- HPV vaccines (Gardasil, Gardasil 9, and Cervarix) reduce the risk of cervical cancer by about 93% and 62% for cancerous or precancerous changes.
- Vaccination is most effective when administered to individuals aged 9 to 26 before infection occurs.
- The duration of vaccine effectiveness and the need for boosters are under ongoing investigation.
- High vaccine costs have raised concerns, prompting countries to consider funding programs for HPV vaccination.
- Japan offers free cervical cancer vaccination for young women since 2010, with specific guidelines from the Ministry of Health.
4. Nutrition
- Vitamin A is associated with a lower risk of cervical cancer.
- Adequate intake of vitamin B12, vitamin C, vitamin E, and beta-Carotene is linked to reduced risk.
5. General Recommendations
- Education about the importance of regular screenings and vaccination plays a crucial role in prevention.
- Initiating screening at age 21 and maintaining regular screenings up to age 65 is recommended in the United States.
- Women over 65 with no abnormal screening results in the previous 10 years and no history of CIN2 or higher may discontinue screening.
- Visual inspection with acetic acid and HPV DNA testing are alternative screening methods, especially in resource-limited settings.
- The effectiveness of Pap tests may vary in developing countries due to challenges such as inadequate healthcare infrastructure and limited resources.
Epidemiology of Cervical Cancer
We have listed the Epidemiology of Cervical Cancer below-
- Globally, cervical cancer is the fourth-most common cancer and cause of cancer-related deaths in women.
- In 2018, an estimated 570,000 new cases and over 300,000 deaths occurred due to cervical cancer.
- Cervical cancer is the second-most common cancer specific to females, following breast cancer.
- It constitutes approximately 8% of both total cancer cases and cancer-related deaths in women.
- Around 80% of cervical cancer cases are reported in developing countries, indicating significant disparities.
- Cervical cancer is frequently detected during pregnancy, with an occurrence of 1.5 to 12 cases per 100,000 pregnancies.
- Mortality rates vary globally, emphasizing disparities in healthcare access and resources.
- The high prevalence in developing countries underscores the need to address healthcare inequalities.
- Cervical cancer’s impact on reproductive health necessitates integrated maternal health and cancer care services.
- Ongoing challenges in resource-limited settings highlight the importance of global initiatives for prevention, screening, and treatment.
Cervical Cancer Key Facts – Important Facts about Cervical Cancer
We have listed the Key Facts about Cervical Cancer below-
| Attributes | Information |
| Location and Types | Cervical cancer can manifest as Squamous cell carcinoma, adenocarcinoma, or other types. An example of normal and abnormal cells can be observed in affected areas. |
| Specialty | Falls under the Oncology specialty. |
| Symptoms | Early stages often present with no symptoms. Later stages may include vaginal bleeding, pelvic pain, and pain during sexual intercourse. |
| Onset and Diagnostic Method | Development spans over 10 to 20 years. Diagnosed through cervical screening followed by a biopsy. |
| Causes and Risk Factors | Human papillomavirus infection (HPV) is the primary cause. Risk factors include smoking, weak immune system, early sexual activity, birth control pills, and multiple sexual partners. |
| Prevention | Regular cervical screening is crucial. HPV vaccines offer preventive measures. Safe sexual practices, including condom use and sexual abstinence, are recommended. |
| Treatment Options | Treatment involves surgery, chemotherapy, radiation therapy, and immunotherapy. |
| Prognosis | Five-year survival rates vary globally: 68% in the United States and 46% in India. |
| Frequency and Deaths (2020) | 604,127 new cases reported globally in 2020. 341,831 deaths attributed to cervical cancer in the same year. |
FAQs on Cervical Cancer
Question-1: What is cervical cancer?
Answer. Cervical cancer is a type of cancer that originates in the cervix, the lower part of the uterus, often caused by the human papillomavirus (HPV).
Question-2: Why is cervical cancer in the news recently?
Answer. Cervical cancer gained recent attention due to the unfortunate demise of Poonam Panday, a well-known star and social media influencer, on February 2, 2024, from this cancer. Her case highlights the importance of awareness, early detection, and ongoing efforts in the fight against cervical cancer.
Question-3: What are the common symptoms of cervical cancer?
Answer. Early stages may not show symptoms, but later stages can include vaginal bleeding, pelvic pain, and pain during sexual intercourse.
Question-4: What are the risk factors for cervical cancer?
Answer. Risk factors include HPV infection, smoking, weak immune system, early sexual activity, birth control pills, and having many sexual partners.
Question-5: How is cervical cancer diagnosed?
Answer. Diagnosis typically involves cervical screening, commonly known as a Pap test, followed by a biopsy to confirm abnormalities.
Question-6: Can cervical cancer be prevented?
Answer. Yes, regular cervical screening, HPV vaccines, and safe sexual practices, such as condom use and sexual abstinence, are preventive measures.
Question-7: What are the treatment options for cervical cancer?
Answer. Treatment may involve surgery, chemotherapy, radiation therapy, and immunotherapy, depending on the stage of the cancer.
Question-8: What is the prognosis for cervical cancer?
Answer. The five-year survival rate varies, with around 68% in the United States and 46% in India.
Question-9: How common is cervical cancer globally?
Answer. In 2020, there were approximately 604,127 new cases and 341,831 deaths worldwide due to cervical cancer.
Question-10: What role does HPV play in cervical cancer?
Answer. HPV infection is a significant cause of cervical cancer, with certain high-risk strains, like HPV 16 and 18, contributing to a substantial number of cases.
Question-11: At what age should cervical screening begin?
Answer. Screening guidelines vary, but generally, it is recommended to start between the ages of 21 and 30, with the frequency depending on factors like risk and previous results.
Question-12: What is Yoga for Cervical Cancer?
Answer. Don’t do Yoga to Prevent Cervical Cancer, It won’t work. If you have found Symptoms of it, go to the Doctor, not on Yoga Matt.